Microbiome’s Role in Patient Care: Advances, Challenges, and Pharmaceutical Opportunities
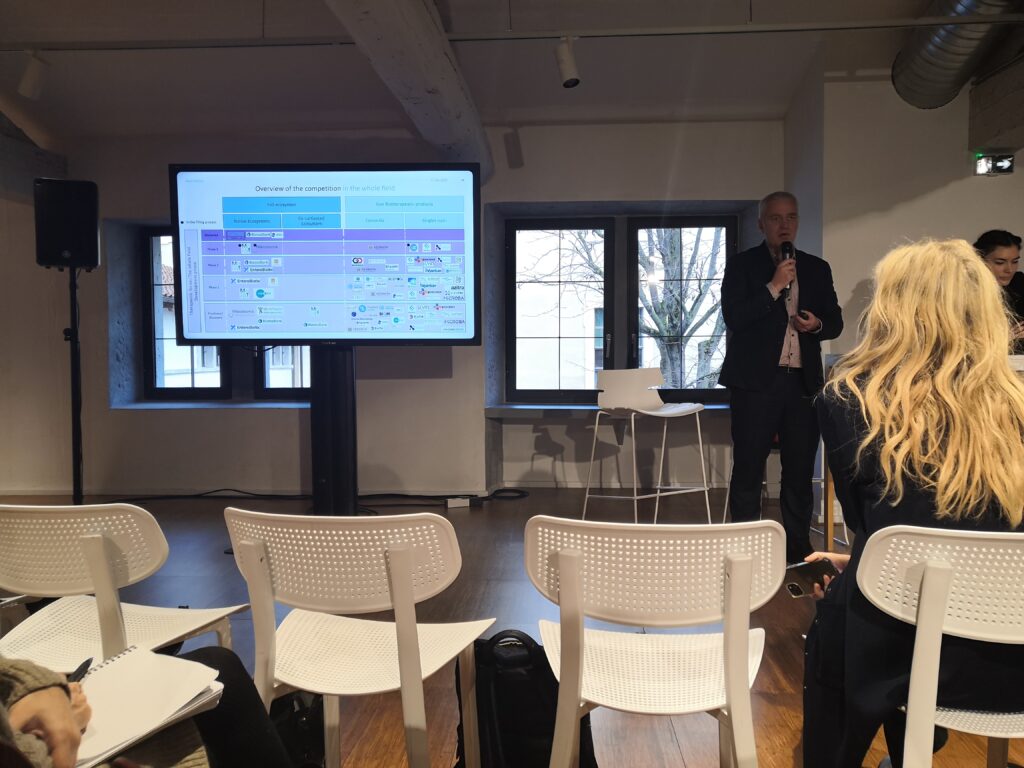
The human microbiome is increasingly pivotal in patient care, particularly in drug development and clinical treatments. Its intricate balance affects health outcomes, treatment efficacy, and disease progression. As bioinformaticians, we are uniquely positioned to decode these complex relationships, providing valuable insights into drug development and patient care. These insights were recently shared at the Journée Microbiotes et Santé 2025 in Lyon, where experts highlighted the intersection of patient care, drug development, and regulatory challenges.
Restoring a Healthy Microbiome: Key to Patient Health
Restoring a healthy microbiome is vital in treating conditions like gastrointestinal disorders, cancer, and immune diseases. One such approach, developed by MaaT Pharma, helps assess microbiome composition and predict cancer treatment outcomes by identifying dysbiosis (microbial imbalance) and eubiosis (balance of beneficial microbes). A balanced microbiome has been shown to improve treatment efficacy, especially in immunotherapy, contributing to better survival rates and fewer adverse effects.
For drug developers, this highlights the need to optimize formulations to complement individual microbiomes, ensuring more effective and better-tolerated treatments. Microbiome-based therapies now follow four key approaches:
- Native products derived from donor microbiomes,
- Co-cultivation therapies using donor-derived microbial communities,
- Consortia-based treatments, which use a subset of microbial species, and
- Single-strain therapies, which leverage specific bacterial strains for targeted interventions.
With over 300 companies worldwide working on microbiome therapies related to oncology —4500 jobs in France alone— competition is intensifying. Industry leaders have already introduced microbiome-based treatments, with costs ranging between $9,000 and $17,000 per course, raising important questions about accessibility and affordability.
Microbiome-Based Therapies in Clinical Trials
Microbiome data is becoming essential in clinical trials, especially for therapies that involve microbial intervention. Single-strain therapies are an example, aiming to restore microbiome balance in conditions like gastrointestinal motility disorders. These therapies also benefit from the growing understanding of the gut-brain axis, linking microbiome health to neurological function.
However, the variability in microbiome compositions across individuals presents challenges for clinical trials. This requires tailored treatment approaches, with bioinformatics and genomic sequencing playing a critical role in identifying patient-specific microbiome signatures and predicting outcomes.
Regulatory Challenges in Europe
The regulatory landscape for microbiome-based therapies in Europe is evolving. The regulatory agencies are working to develop frameworks for assessing these treatments, with a particular focus on SoHO (Substances of Human Origin) regulations, which now govern microbiome-based therapies. A major challenge remains the lack of established biomarkers and the microbiome’s inherent variability, complicating the clinical validation of therapies. As a result, regulatory approval can be complex, with a need for more precise diagnostic tools and standardized testing methods.
In contrast, while the US FDA has approved some microbiome therapies, European regulators remain more cautious, emphasizing safety and efficacy before market approval. With drug evaluations shifting from national-level approval to European-level assessment, ensuring a streamlined yet rigorous process will be crucial for industry growth.
Patient-Centric Microbiome Research
A notable shift in clinical research is the increasing focus on patient-centered models, where patients are active participants in the research process rather than passive subjects. This evolution is essential for ensuring broader acceptance of microbiome therapies while addressing concerns related to cost, accessibility, and long-term effects. Studies now highlight the need for financial compensation, ongoing support, and patient education to enhance engagement in clinical trials.
Furthermore, patient perspectives are reshaping research priorities, influencing everything from trial design to treatment acceptability. The growing involvement of patients ensures that microbiome-based research remains relevant and impactful, ultimately leading to better healthcare outcomes.
Conclusion
The microbiome represents an exciting frontier in healthcare, offering transformative potential for both drug development and patient care. For bioinformaticians, this means decoding complex microbial ecosystems to inform clinical treatments. As research progresses, integrating microbiome data into clinical trials, overcoming regulatory challenges, and embracing patient-centered approaches will lead to more targeted, effective treatments for the future.